Changing COVID-19 Age Demographics Illustrated By EMS Data
As the United States braces for what appears to be the anticipated “second wave” of COVID-19 cases, EMS professionals continue to work diligently on the front lines. Now, more than eight months into the most drastic spike of cases in the U.S., EMS call data is more clearly revealing new characteristics of the virus, including negating the widespread belief that the virus only impacts an older population.
What EMS Agencies Are Observing on Calls
Since March 2020, ESO has been maintaining a COVID-19 data dashboard based on EMS surveillance data. The online dashboard features a series of snapshot reports and graphs based on data obtained from the ESO database, consisting of more than 2,600 EMS agencies across the U.S., and updated daily.
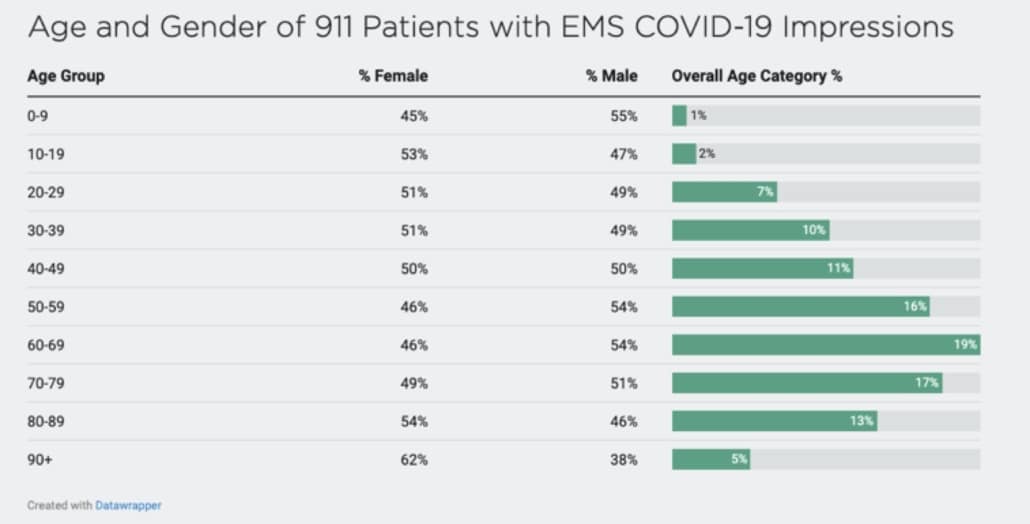
Among the numerous trends and variables, a key metric tracked on the dashboard is “Encounter and Demographic Characteristics for Patients with EMS COVID-19 Impressions,” specifically looking at the age and gender of 9-1-1 patients with COVID-19 impressions.
While the data does fall in line with the assumption that COVID-19 is a disease that disproportionately impacts seniors and those with underlying medical conditions, a concerning statistic is that 47% of COVID-19 patients were actually under the age of 60.
What It Means For Younger People
Recent studies cited by the AMA indicate a shift in the median age for COVID-19 cases, dropping from age 46 in May down to age 37 in July. Additionally, researchers have observed that increases in the number of COVID cases for younger age groups are often closely followed by a rise in positive COVID-19 tests for older populations in the same communities. This suggests that while the illness does not seem to impact younger Americans as dramatically, it may be directly accountable for a subsequent spread to more vulnerable populations.
Additionally, as observed in a recent JAMA Internal Medicine Editor’s Note, while young adults are much less likely than older persons to become seriously ill from COVID, if they reach the point of hospitalization, their risks are still substantial. Also, obesity and hypertension put patients of all ages at greater risk, especially males. Since these health conditions are preventable and treatable, reducing serious COVID-19 risks is an additional motivation to practice healthy diets and increase exercise.
CDC COVID-19 Data and Demographics
The U.S. Centers for Disease Control and Prevention (CDC) continues to collect and monitor a wide range of demographic information from COVID-19 patients, explaining that race and ethnicity are risks are often tied to other conditions that impact health, such as socioeconomic status, access to health care, and increased exposure to the virus due to certain occupations.
In a recent report on Coronovirus data looking at rates of positive tests, hospitalization, and death by race, the CDC found the following trends (when comparing other races to “white, non-Hispanic persons”):
- Black or African Americans were 2.1x higher risk for death
- American Indian or Alaska Natives were 5.3x higher risk for hospitalization
- Hispanics or Latinos were 4.6x higher risk for hospitalization
Across the board, all other races were 1-3x more at risk for testing positive for COVID and an almost 5x higher risk for hospitalization (with the exception of Asian persons who were still a 1.3x higher risk). The CDC tied these increases back to factors that increase community spread and individual risk: crowded situations, close physical contact, enclosed spaces, and duration of exposure. Many of these risk factors are increased from specific occupations such as frontline, essential, and critical infrastructure workers.
The Coronavirus Continues to Spread Regardless of Age
While older populations continue to lead the demographics in number of cases, hospitalizations, and death, the age shift does paint a more concerning picture for younger Americans. The CDC cites that cases of COVID-19 in individuals aged 18–22 years increased by 55% between Aug. 2 and Sept. 5, 2020. Additionally, the number of instances of COVID-19 reported between June and August 2020 was highest in the age group 20–29 years, accounting for more than 20% of the total. This differs dramatically from the pandemic’s early days when the incidence was highest in older adults aged at least 60 years.
Reducing the Coronavirus’ Spread
The CDC and other government officials are continuing to beat the drum of prevention to the general public, encouraging them to continue vigilance in wearing masks, social distancing of at least 6 feet, practicing good hand hygiene, and cleaning and disinfecting. Ideally, the concept that COVID-19 is only a threat to older Americans will soon be discarded, and all age groups will be able to practice a higher level of vigilance to prevent further spread as much as possible in the months to come.
To see more EMS data relating to COVID-19 impressions, visit the ESO Data Dashboard.
Download the ESO 2020 EMS Index: Special COVID-19 Edition, focusing on 911 calls, Personal Protective Equipment (PPE) usage, and other metrics related specifically to COVID-19.